Provider Update | Spring 2025
Tuesday, Apr 29, 2025We’re bringing you the latest news for health, dental and pharmacy providers. Read on for information on appropriate billing, an update on dental claims submissions, how to download our paperless predetermination forms, and answers to frequently asked provider questions!

Appropriate billing for high-cost drugs
At Pacific Blue Cross, our guiding principle for drug benefit management is ensuring our members have access to the right medications at the correct dosage.
A recent review of several high-cost drugs (listed below) found that PharmaCare limits reimbursement based on a daily price. To ensure accurate billing for these and future high-cost drugs, we have aligned with this approach.
|
Example: Appropriate billing for Skyrizi, when used to treat plaque psoriasis |
|
|
Common Billing Errors |
Appropriate Billing Process |
|
Submit initial claim for 1-day supply |
Submit initial claim for 28-day supply |
|
Copy refills from original prescription using a 28-day supply |
Submit refills from original prescription using 84-day supply |
These mistakes can lead to inaccurate PharmaNet records and incorrect PharmaCare reimbursement.
To ensure proper billing, we are updating our system to reimburse high-cost drugs according to the doses approved by Health Canada and the calculated daily reference price. If a claim for these drugs is submitted with an incorrect day supply, reimbursement will be limited to the appropriate dose, and the following return message will appear:
“Dosage exceeds maximum allowable. We have considered the drug cost portion up to the appropriate maximum dose considered under the plan.”
List of high-cost drugs*:
- Bimzelx
- Camzyos
- Emgality
- Entyvio
- Kerendia
- Kevzara
- Nucala
- Omvoh
- Prevymis
- Qulipta
- Skyrizi
- Tezspire
- Uptravi
- Verquvo
- Zeposia
*Please note: This policy will also apply to future high-cost drugs.
If you have any questions, please feel free to contact our Customer Service Representatives by calling 604 419-2000 or 1 877 PAC-BLUE.
It is crucial that the day supply submitted for each claim accurately reflects the prescribed dosage to maintain both PharmaNet records and claims payment accuracy.
Dental claims submission update: Fax option discontinued

We are pleased to share that our claims processing is running smoothly and efficiently, with submissions being handled within the expected turnaround times.
As a result, the temporary fax submission option – introduced as a short-term measure to address increased processing times – has been discontinued and is no longer be available. To ensure timely processing of your claims, please use our regular submission channels.
We appreciate your cooperation and thank you for trusting us with your health benefits needs. If you have any questions or need assistance, please contact customer service by calling 604 419-2000 or toll-free at 1 866 PAC BLUE.
.
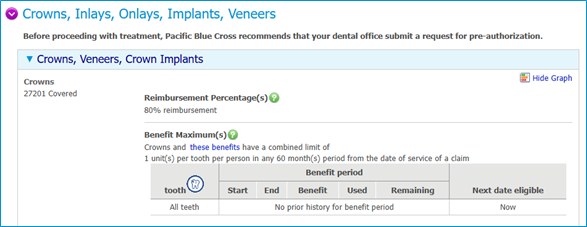
Accessing your patient’s dental plan breakdown

Did you know you can look up your patient’s plan breakdown in PROVIDERnet?
- Click on the Eligibility tab.
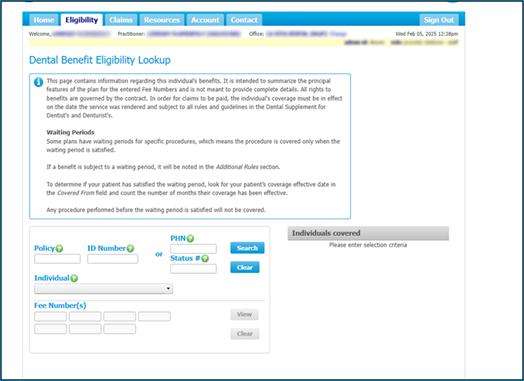
- Enter the member’s policy and ID number, and search by specific fee codes to view coverage details.
Predetermination statements are now paperless!

We’ve gone paperless for health and dental provider predetermination statements. This transition is part of our efforts to reduce paper waste and enhance security.
Providers registered with PROVIDERnet and using direct deposit can now download statements directly in PROVIDERnet. Simply log into your PROVIDERnet account, click Claims and select Statements. Filter by “Predetermination Statements”, select the appropriate “Provider Location” and filter by date. Click View to download the PDF format.
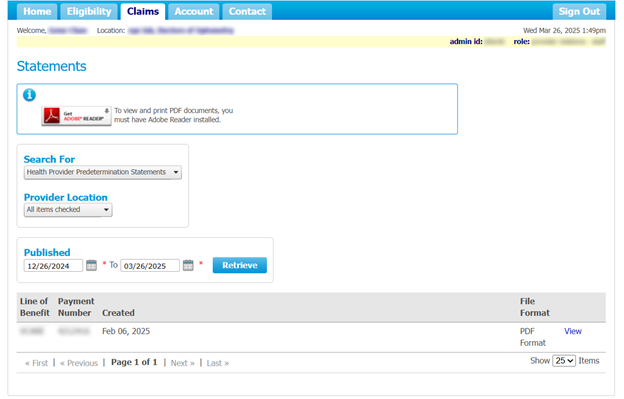
Dental providers, please note this change only applies in cases where a predetermination is typically submitted for your patients, including those on the MSDPR and FNHA plans.
Physiotherapy Frequently Asked Questions

We recognize the importance of physiotherapy and want to provide further clarity on coverage.
To support plan members and providers of this benefit, we have enhanced the Pacific Blue Cross Physiotherapy Frequently Asked Questions.
Provider Frequently Asked Questions
Who can set up direct deposit for my provider office?
Only the primary administrator for your provider office can set up direct deposit.
- For dental providers, this is the dental practitioner.
- For health providers, this would usually be the office manager or front desk staff.
- For pharmacy providers, this is the pharmacy owner.
Will I continue to receive paper statements once I sign up for direct deposit?
No. After enrolling for direct deposit, you will no longer receive paper statements. All statements will be available online, through your PROVIDERnet account.
Why are my Ministry claims getting rejected?
Submitting multiple pre-determinations for the same claim will result in an adjudication error. Please submit only one pre-determination per claim.
Why am I not able to find my patient’s pre-determination?
Please ensure you are viewing the provider location that the patient’s pre-determination was approved under. Navigate to Authorized Products and Services and select Change to make sure the correct location is selected.
Does Pacific Blue Cross register out-of-province providers?
Yes, we register out-of-province dental and pharmacy providers.
Still have questions? Visit Provider Resources.
Set up your PROVIDERnet account and direct deposit

PROVIDERnet enables secure, weekly direct deposit payments directly into your bank account – eliminating cheque delays and manual processing.
With PROVIDERnet, you can also:
- Submit pre-determination requests (if applicable) and view pre-determination results online (if applicable)
- Access claims statements instantly
If you haven’t registered for PROVIDERnet yet, take a few minutes to do so now. Visit PROVIDERnet or check out our step-by-step video.
For primary administrators:
Add direct deposit details for faster, more secure payments. To set up direct deposit:
- Sign in to PROVIDERnet.
- Head to the Account tab and select Direct Deposit.
- Add your direct deposit information.
For additional instructions, watch How to set up direct deposit in PROVIDERnet.
We Want to Hear from You!
Have a topic or idea you'd love to see in Provider Updates? Share your suggestions with us at provider@pac.bluecross.ca and help us make future editions even better!