Frequently Asked Questions (FAQs)
Plan members joining My PBC Benefits
General Inquiries
-
What is My PBC Benefits?
Powered by TELUS AdjudiCare, My PBC Benefits is the Pacific Blue Cross claim administration platform for national members. Through My PBC Benefits, you can submit claims online, view your benefit coverage, check claims history, verify remaining balances for your benefits plan, access Explanation of Benefits statements, and find documents and forms associated with your benefit plan.
-
As a new member to My PBC Benefits, will I receive a new benefits ID card?
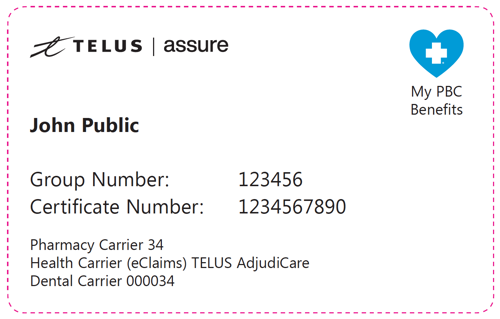
Members joining My PBC Benefits will receive a My PBC Benefits/TELUS Assure member ID card in the mail. Please use the numbers on the card when you or your dependents visit a health care provider (pharmacists, dentists, or paramedical practitioners), and when you submit a claim for reimbursement.
A digital copy of your ID card is also available through the My PBC Benefits portal or mobile app.
-
How do I register for My PBC Benefits?
My PBC Benefits can be accessed through the online portal and/or the mobile app.
Online portal: Register to the online portal
Mobile app: Download and register for the mobile app
For more information on how to use My PBC Benefits, please refer to the My PBC Benefits User Reference Guide.
-
Do I need to let my health care providers (i.e., pharmacists, practitioners, dentists) know that I have a new benefits ID card?
Yes, please show your new card to providers that submit claims online on your behalf (i.e., pharmacists, dentists, paramedical practitioners like optometrists, massage therapists, chiropractors or physiotherapists).
Providers with direct billing can submit claims online on behalf of My PBC Benefits members at providerportal.telushealth.com. New providers will need to register for TELUS AdjudiCare (My PBC Benefits software provider) at telushealth.co/eclaims.
-
How do I set up direct deposit in My PBC Benefits?
Once you have registered to My PBC Benefits, you can set up your banking information by logging into the portal or the mobile app. Click the person icon in the top-right menu and then select Direct Deposit.
For more information on direct deposit and other My PBC Benefits features please refer to the My PBC Benefits User Reference Guide.
-
Where can I find a claim form if I need to send my claims through mail?
Please refer to the Forms and Resources section on this page to find Health, Dental and Drug claim forms.
-
Who should I reach out to if I have questions or concerns about my benefits or claims?
My PBC Benefits members will have access to dedicated phone numbers to contact the Pacific Blue Cross call centre. You can also send us a message using the form below:
- Toll-free: 1 866 366-0430
- Lower Mainland: 604 419-2381
- Available during business hours from 8:00 am to 4:30 pm PST, Monday to Friday.
- Contact form: pac.bluecross.ca/mypbcbenefits-contactus
- Toll-free: 1 866 366-0430
Claims Processing Information
-
How do I submit a claim?
You can submit your claims online through the My PBC Benefits portal or mobile app.
Through My PBC Benefits, you can view your benefit coverage, check claims history, verify remaining balances for your benefits plan, access Explanation of Benefits statements, and find documents and forms associated with your benefit plan.
For more information on how to submit a claim, please refer to the My PBC Benefits User Reference Guide.
-
How long does it take for my claims to be processed?
Claim processing times may vary depending on the submission method and whether the claim was submitted by the member or the provider.
For most claims submitted online or through the mobile app, payments are processed within the next business day, when direct deposit is set up. For claims submitted by mail, the standard turnaround time is seven days for members and ten days for providers.